Dental Insurance Verification: The Complete Guide to Faster, Cleaner Eligibility Checks and Better Collections
Dental insurance verification is one of the most time-consuming workflows in dentistry, and its impact goes well beyond scheduling. It affects collections, patient trust, and staff burnout. CAQH’s benchmarking shows eligibility and benefits verification is also a major driver of dental administrative spending.
This guide breaks down what dental insurance verification involves, why portal-driven workflows break down, and what a modern, automated eligibility process looks like.
What Is Dental Insurance Verification?
Dental insurance verification is the process of confirming a patient’s coverage details before treatment, including whether coverage is active, what services are covered, plan limitations, and what the patient is likely to owe.
CAQH defines eligibility and benefit verification as an inquiry from a provider to a plan to obtain eligibility, coverage, or benefits, and the plan’s response. This is commonly exchanged via the ASC X12N 270/271 standard.
Why it matters: CAQH notes that broader adoption of fully electronic eligibility checks can help give patients clarity before and at the time of service, reduce surprise bills, and support more informed decision-making.
The Real Cost of Verification in Dental
Eligibility verification is not “just a front desk task.” It is measurable in dollars and minutes, and it is one of the largest operational cost centers in dental administration.
- Eligibility and benefit verification spending rose to $2.1B in 2023, and eligibility and benefits represent the largest portion of annual dental administrative spend at 30%.
- Portals drive cost and complexity. CAQH highlights that variations in portal requirements and formats add complexity and labor.
- The savings opportunity is large. CAQH estimates the dental savings opportunity from moving remaining manual and portal checks to fully electronic workflows is $580M annually.
- Time adds up quickly. CAQH’s dental benchmarking shows a meaningful time savings opportunity per check when shifting from manual or portal-based modes to fully electronic transactions.
What to Verify in Dental: A Practical Checklist to Prevent Rework
A strong verification process does not just confirm coverage. It prevents downstream issues.
1) Coverage status and effective dates
- Active vs inactive coverage
- Effective date and termination date
- Subscriber vs dependent eligibility
2) Plan type and network rules
- PPO vs DHMO/DMO
- In-network vs out-of-network status
- PCP or referral requirements (if applicable)
3) Benefit structure
- Preventive, basic, major coverage percentages
- Annual maximum remaining
- Deductible and deductible remaining (individual and family)
- Waiting periods (major, ortho)
- Frequency limitations (exams, prophy, bitewings, perio maintenance)
- Missing tooth clause
- Downgrades or alternate benefits (example: composite vs amalgam, crown downgrades)
4) Procedure-level specifics for scheduled care
- Coverage for the CDT codes you plan to bill
- Whether documentation is required (narrative, x-rays, perio charting, intraoral photos)
- Whether prior authorization or pre-determination is recommended
5) Coordination of benefits and secondary coverage
Secondary coverage often introduces more manual work and unclear outputs. Even if you do not fully coordinate benefits at verification time, flagging secondary coverage early reduces downstream surprises.
6) Patient financial responsibility
Use verification output to set:
- A conservative estimated patient portion
- Payment timing (example: collect day of service for estimated portion)
- What happens if the plan pays less than expected
The Most Common Verification Workflows, and Where They Break
Most practices use a mix of:
Fully manual (phone, fax, email)
Slow, inconsistent, and hard to scale.
Web portals (partially electronic)
CAQH classifies portal workflows as “partially electronic.” They can feel digital, but they are labor-heavy because they require human navigation and transcription, and portal variability adds complexity.
Fully electronic (standard transactions)
For eligibility, “fully electronic” commonly means 270/271 transactions.
Where they break most often: returned information can be incomplete, not procedure-specific, or hard for staff to interpret. That drives teams back into portal hopping and phone calls.
How Better Verification Improves Collections Without Guessing
Revenue cycle outcomes are shaped upstream. When verification is clean and consistent:
- Fewer surprise balances lead to less patient pushback
- More accurate estimates support stronger day-of-service collections
- Fewer eligibility issues lead to fewer resubmissions and follow-ups
CAQH reports denial rates across healthcare remain a material issue, reinforcing why “right-first-time” administrative data matters.
What “Good” Looks Like: The Modern Dental Verification Standard
A high-performing verification process has five characteristics:
- Automated where possible, minimizing human navigation
- Procedure-aware, mapping benefits to scheduled care
- Trustworthy, producing clean, predictable outputs with fewer exceptions
- Documented, with consistent storage and notes for auditability
- Operationalized, with repeatable SOPs and an exception workflow
This is where teams win time back. CAQH’s benchmarks show a clear time savings opportunity when practices move away from manual and portal-heavy modes.
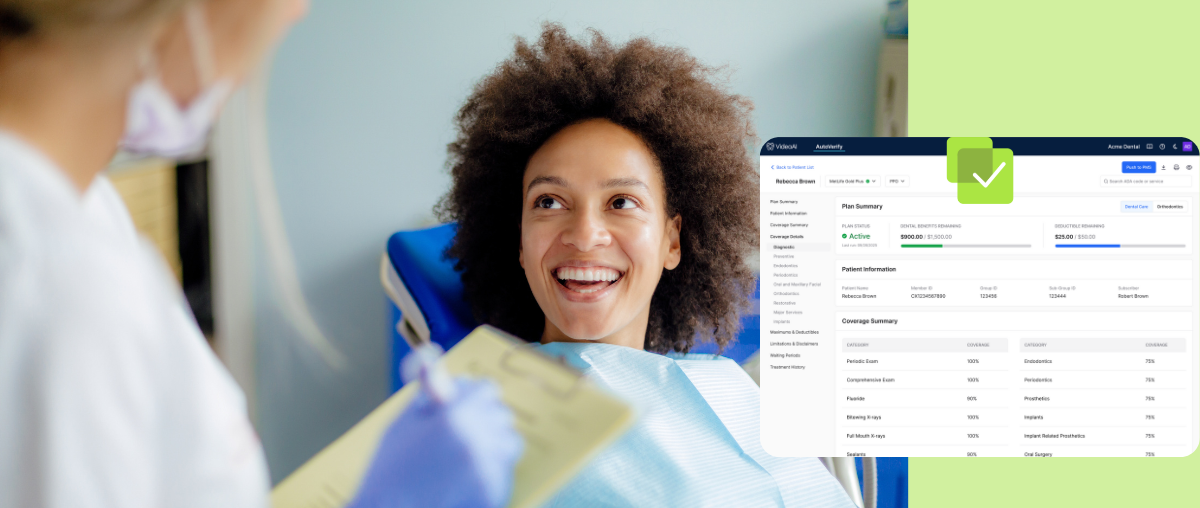
AutoVerify: Eligibility Checks You Don’t Have to Double-Check
AutoVerify is VideaAI’s automated dental insurance verification solution. It confirms eligibility and key benefits before every appointment, standardizes results into an easy-to-read format, and flags issues early, so teams spend less time in portals and more time focused on patients.
Learn more here.
Why Automation Matters at Scale
CAQH estimates the dental industry conducted 1.2 billion eligibility and benefit verifications in 2023, and these checks represent a significant share of overall dental administrative transaction volume.
With eligibility and benefits representing the largest portion of dental administrative spend at 30%, the upside of a cleaner, more automated workflow is measurable in both dollars and staff time.
If you want a tool focused on reliable, dental-usable verification that reduces manual portal work, you can learn more about AutoVerify.
FAQs
What is the difference between eligibility and benefits in dental insurance?
Eligibility confirms a patient is active on a plan and covered. Benefits detail what the plan pays for categories or procedures, plus limitations like frequency, waiting periods, and maximums.
How long should dental insurance verification take?
CAQH benchmarking shows fully electronic transactions are meaningfully faster than manual and portal-driven modes, with a clear per-check time savings opportunity when practices switch to fully electronic workflows.
Why do dental offices still use insurance portals?
Portals can be the only place to view certain details, but CAQH notes portal requirements and formats vary, adding complexity and cost.
How big is the dental eligibility verification workload?
CAQH estimates the dental industry conducted 1.2 billion eligibility and benefit verifications in 2023.
More articles
Subscribe to Dental AI Hub
Be the first to know about releases and industry news and insights.

%20copy.png)